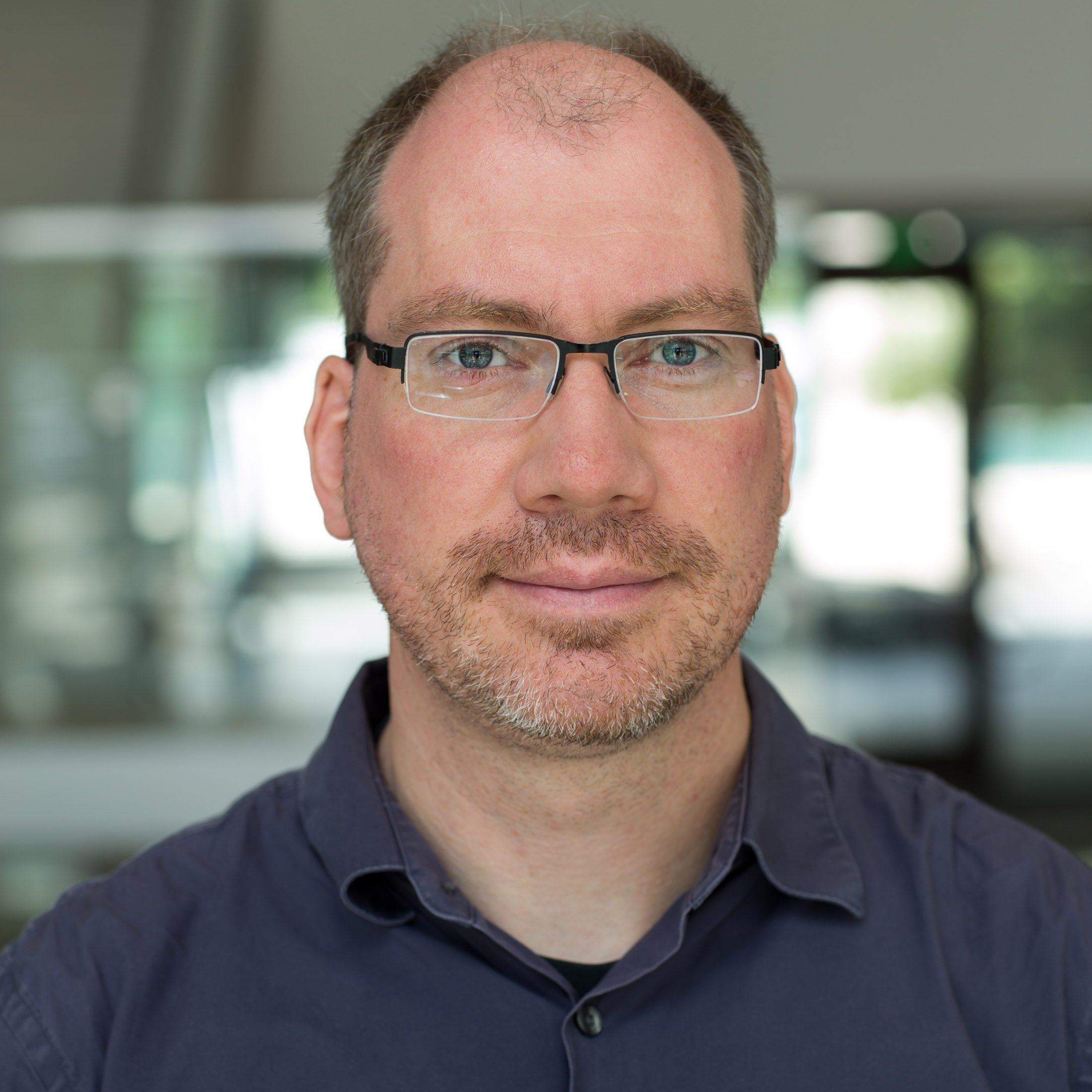
Alumni Profile: Dr. Tim Henrich ‘96
Dr. Timothy Henrich today. (Source: UCSF Department of Medicine website)
Before starting his illustrious career in medicine, Dr. Timothy Henrich was an Oberlin Shansi fellow in Machida, Japan. In this profile, we caught up with Tim, learning more about his groundbreaking research on HIV, SARS-CoV-2, and human herpes viruses, his path to becoming a physician scientist, his philosophy of optimism, and his years of support to Shansi as our resident expert for the Fellows’ pre-departure medical briefing.
We often tell current and prospective Fellows that a Shansi Fellowship can lead to a host of careers, including medicine. You are a prime example of this! Could you let us know how you went from teaching English at J.F. Oberlin University to a career in medical research? How did your time at JFOU contribute to this professional path?
Tim: Ha! Great question. In true Oberlin fashion, I initially was planning on a career in Archeology (I also studied trumpet at the Conservatory on the side), but wanted to have an experience living in a culture very different from my own and to become proficient in a second language. Hence Shansi. I loved teaching but I realized as the Returned Fellow following my time in Tokyo that I still loved science. Medicine seemed like a great way to combine science and research with social justice. It also requires interpersonal communication — all things that I thought I wanted to have in a career.
My experiences at Obirin (the previous old name of J.F. Oberlin back then) really drove home my passion for teaching, which I now do daily in my profession, teaching medical students, fellows and residents in the clinic and on the wards, mentoring graduate students, post-docs and junior researchers, etc.
Could you tell us about your current work and research at UCSF?
I am a physician scientist and run a translational infectious disease research group with a focus on HIV, SARS-CoV-2 and Human Herpes Viruses. I am also an infectious disease clinician that specializes in treating immunocompromised patients with cancer, HIV, and stem cell and solid organ transplants at UCSF Medical Center. I also treat immunocompromised patients with COVID-19. My research has several main components:
Studying how HIV persists throughout the body despite antiretroviral therapy and running pathogenesis-based human studies using immune modifying agents, gene therapy and stem cell transplant to achieve a cure for HIV (i.e., eliminating latent HIV reservoirs in tissues)
Implementing novel technologies to study persistence of viruses in tissues (HIV, SARS-CoV-2) such as immunoPET imaging (using PET scanners with radiolabeled tracers that allows us to visualize viral proteins across the entire body in 3D, without any invasive tissue biopsies) and using PET imaging to track immune cell activation, trafficking throughout the body and function. I also work closely with tissue from living participants as well as with autopsy specimens from people with HIV and/or recent SARS-CoV-2 infection who died of sudden death to determine "multi-omic" (e.g. gene expression) virus-host immune responses, how viruses persist in tissues and how they escape immune clearance.
Overseeing the UCSF LIINC [Long-term Impact of Infection with Novel Coronavirus] cohort which is a study of >750 people recovering from COVID-19 that either have persistent symptoms ("Long-COVID") or have complete recovery to understand why some people develop post-viral syndromes.
Implementing anti-viral and immune modifying therapies to treat people with Long-COVID.
Discovering novel biomarkers of viral infection for either diagnostics or for targeting anti-viral therapies.
How did your research working towards a cure for HIV inform your research about the long-term effects of COVID-19?
This is a fascinating question! When the pandemic was fast approaching, we rapidly realized that SARS-CoV-2 was not an ordinary virus and that there were likely to be profound sequelae not just during acute infection but during convalescence as well. Our HIV research was initially put on hold during the early lockdown in 2020 and we realized that we already had the existing infrastructure (clinical, laboratory, epidemiological) to rapidly retool our activities to study SARS-CoV-2. We were able to leverage existing NIH funding as well as corporate and non-profit funding to rapidly expand our LIINC cohort.
Unlike most other academic scientific endeavors, we felt that any science around COVID-19 should be collaborative and in the public domain and we used LIINC to support over 40 groups across the world to perform cutting edge research into long COVID and immune sequelae of infection. The past three years were a wild ride and emotionally draining. For example, I was juggling treating patients with acute COVID, even prior to vaccination, [which was the first time in my life I felt that my work could actually put my life and the wellbeing of my family and colleagues at risk] with trying to rapidly expand our LIINC research infrastructure. The research was exhilarating but mixed with the pain of seeing so much morbidity and death in our patient population, especially during the initial waves.
Addressing your actual question: There is huge overlap between studying HIV persistence and cure strategies and post-acute sequelae of COVID-19. The tools are essentially the same and it was a no brainer to expand rapidly to counter the emerging global pandemic.
Dr. Tim’s annual medical advice Zoom session.
You’ve been helping Shansi with orientation for the past several years, preparing new Fellows with medical info of what they’ll face while living and traveling in Asia. What do you wish you’d known as a new Fellow who was preparing to go live abroad?
Ha! Hindsight is always 20/20 of course, and there are so many things I wished I had known. But I was also 22 years old, naïve, inexperienced but full of curiosity. I think if I had a better understanding that life will always bring challenges and surprises, that would have been nice, but you only learn this by experiencing it.
In two different interviews I’ve seen of yours, you mention how you are an optimist. How does your attitude and the attitude of the researchers with whom you collaborate impact the work that you do?
Great question! I think you have to be an optimist in my profession and do the work that we do and not self-implode. The clinical care and research can be challenging and always unpredictable. Many of my colleagues are also optimists but also retain a grounding sense of humor and reality about the world. My job is all about collaborating with researchers, clinicals, students, patients, patient families, etc. and we are who we surround ourselves with.
Dr. Timothy Henrich stands in a grocery store in Japan with co-fellow Viet Ngo in 1995, during his two year fellowship.